Information on TTTS
TWIN TO TWIN TRANSFUSION SYNDROME
The following information is very medical. You can access guides and videos about TTTS produced for parents here.
Definition and Staging
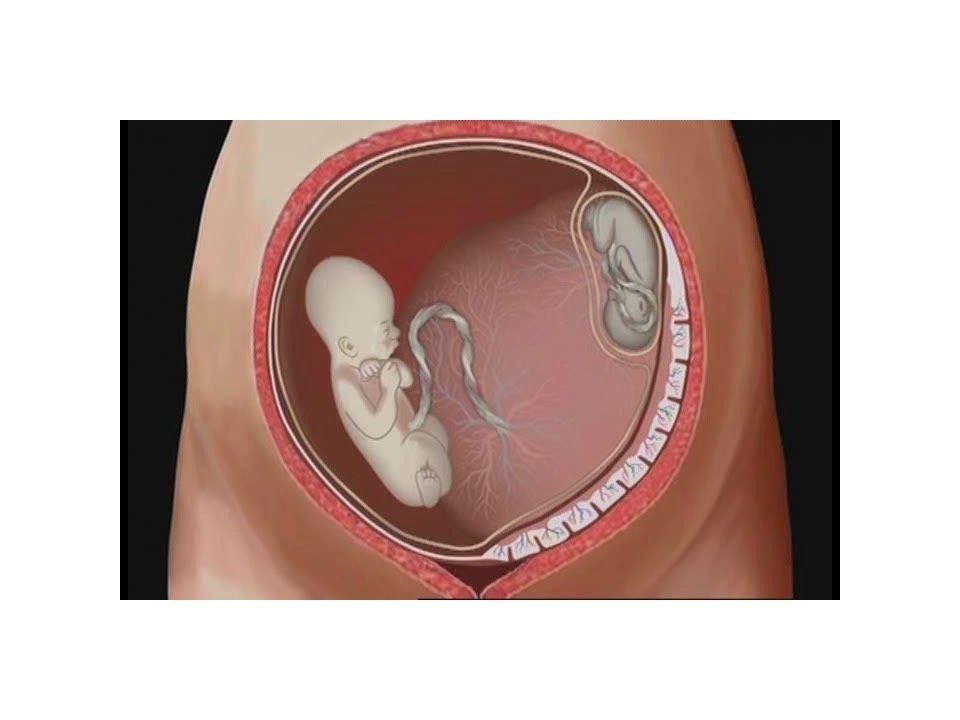
Twin to twin transfusion syndrome (TTTS) is defined as a significant discordance in the amniotic fluid volume within the amniotic sacs of monochorionic diamniotic (MCDA) twins (polyhydramnios oligohydramnios sequence) (Quintero 1999; Quintero 2003; Roberts 2008; Roberts 2014; RCOG in press 2014). The amniotic fluid volume surrounding the ‘donor’ twin has a deepest vertical pocket (DVP) of <2cm (oligohydramnios) and the ‘recipient’ twin has a DVP ≥8cms (polyhydramnios) before 20 weeks and ≥10cm after 20 weeks’ gestation. TTTS is far less common in monochorionic monoamniotic (MCMA) twin pregnancies, compared with MCDA, twin pregnancies, and the ultrasound diagnostic features include polyhydramnios in the common amniotic sac and discordant bladder sizes.
TTTS is associated with increased perinatal mortality and morbidity; if untreated, it leads to fetal demise in 90% of cases, with morbidity rates in survivors of over 50% (Roberts 2008; Roberts 2014; RCOG in press 2014). TTTS is caused by the presence of unidirectional, intertwin, vascular anastomoses on the placenta causing a haemodynamic imbalance between the two twins. The severity of the TTTS is currently defined using the Quintero staging system (Quintero 1999; Quintero 2003), as follows:
• Stage I: polyhydramnios oligohydramnios sequence: DVP >8cm in the recipient & DVP < 2cm in the donor
• Stage II: bladder in the donor twin not visible on ultrasound scan
• Stage III: Doppler velocimetry changes in the umbilical artery or ductus venosus
• Stage IV: Hydrops in one or both twins
• Stage V: Death of one or both twins
However, other investigators have reported that intertwin cardiac dysfunction may be present even in early Quintero stage disease (Raboisson 2004).
Epidemiology
TTTS affects approximately 10% of monochorionic diamniotic (MCDA) twin pregnancies (Visintin 2011; Lewi 2010). The majority of multiple pregnancies complicated by TTTS are MCMA twin pregnancies (95%), with the remainder seen in MCMA twins, DC and MC triplet pregnancies.
The National Institute for Health and Care Excellence (NICE) guideline recommends that all monochorionic twins are screened for TTTS by regular ultrasound scans every two weeks from 16 weeks of gestation (NICE 2011). If TTTS develops, urgent assessment and management by a fetal medicine expert is required (NICE 2011).
Management
Fetoscopic laser ablation is considered the treatment of choice before 26 weeks of gestation; compared to amniodrainage, it is associated with lower rates of fetal loss and disability (Roberts 2008; Roberts 2014). According to published studies, laser ablation resulted in at least one neonatal survivor in over 80% (stage II), 67-83% (stage III) and 50-70% (stage IV) (Quintero 2003; Moise 2005; Senate 2006; RCOG in press 2014). Despite limited evidence, it seems that fetoscopic laser ablation is also the best treatment for TTTS in early-onset (<16 weeks) and late-onset (>26 weeks) disease (Baud 2013; Middeldorp 2007). There are limited data to guide clinical practice, either on the investigation or follow-up of TTTS pregnancies after treatment, or on the timing or mode of delivery.
Less common management options include selective termination of pregnancy using bipolar diathermy or radiointerstitial thermal ablation of one of the umbilical cords (Taylor 2002; Paramasivam 2010). These options are usually reserved for pregnancies complicated by severe TTTS, such as when there is severe growth discordance with the donor twin severely growth restricted, hydrops in the recipient or evidence of cerebral damage in either twin.
The recurrence rate following ‘selective’ fetoscopic laser ablation is 14%, likely due to missed anastomoses. This could potentially be avoided by ‘equatorial laser dichorionization’ (the Solomon) fetoscopic laser technique (Slaghekke 2014). Similarly, cases of twin anaemia polycythaemia sequence (TAPS), reported in up to 13% of cases following laser ablation, were less common when the Solomon technique was used (Slaghekke 2014).
The management of stage 1 TTTS remains controversial. Observational studies are difficult to interpret because of referral bias. This could explain the differences in the reported progression and survival rate in stage 1 TTTS managed conservatively. The disease progression (approximately 35%) is usually unpredictable, with regression in 28%, and a stationary course in 37% of pregnancies. Furthermore, some pregnancies complicated by TTTS progress from stage I to stage III without obviously passing through stage II (Dickinson 2004). The management of stage 1 TTTS remains controversial. An RCT, comparing immediate treatment by fetoscopic laser ablation versus conservative management, is currently underway (Ville 2010). However, recruitment for this study has proven to be difficult so far.
The survival rate and neurodevelopmental outcomes of TTTS cases in the UK are unknown. These cases are usually managed in specialist fetal medicine centres. However, there is no surveillance programme for follow-up of these infants after birth. As a result, data on the survival rates in these fetal medicine centres are not routinely ascertained or reported. There are many unanswered questions in relation to the natural history, optimal management and outcomes of TTTS in the UK.
Establishing a registry of all UK twin pregnancies complicated by TTTS, treated or not, will help to answer these uncertainties. Comparable databases have been set up in the USA and Australia, with initial findings due to be reported soon. A national UK TTTS Registry could provide a tool to assist in improving clinical management and decision making by participating in national quality programs. The registry could also be used for data submission to NHS England, which will soon be an essential requirement for all fetal medicine centres in the UK to ensure that these high-risk pregnancies are receiving the safest high-quality service they deserve. The TTTS registry has the opportunity to improve care at a local, regional, and national level.
Laser ablation surgery performed on identical twins with TTTS
REFERENCES
1. Overview | Twin and triplet pregnancy | Guidance | NICE [Internet]. NICE; 2019 [cited 2023 Apr 19]. Available from: https://www.nice.org.uk/guidance/
2. Management of Monochorionic Twin Pregnancy. BJOG: An International Journal of Obstetrics & Gynaecology. 2017;124(1):e1–45.
3. Khalil A. The rate of twin birth is declining. Ultrasound in Obstetrics & Gynecology. 2021;58(5):784–5.
4. Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol 1999;19:550–5.
5. Lewi L, Gucciardo L, Van Mieghem T, de Koninck P, Beck V, Medek H, Van Schoubroeck D, Devlieger R, De Catte L, Deprest J.Monochorionic diamniotic twin pregnancies: natural history and risk stratification.Fetal DiagnTher. 2010;27(3):121-33. doi: 10.1159/000313300.
6. Khalil A. Modified diagnostic criteria for twin-to-twin transfusion syndrome prior to 18 weeks’ gestation: time to change? Ultrasound Obstet Gynecol. 2017 Jun;49(6):804–5.
7. Khalil A, Rodgers M, Baschat A, Bhide A, Gratacos E, Hecher K, et al. ISUOG Practice Guidelines: role of ultrasound in twin pregnancy. Ultrasound in Obstetrics & Gynecology. 2016;47(2):247–63.
8. Murgano D, Khalil A, Prefumo F, Mieghem TV, Rizzo G, Heyborne KD, et al. Outcome of twin-to-twin transfusion syndrome in monochorionic monoamniotic twin pregnancy: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2020 Mar;55(3):310–7.
9. Ville Y. Twin-to-twin transfusion syndrome: time to forget the Quintero staging system? Ultrasound Obstet Gynecol 2007;30:924–7.
10. Mustafa HJ, Javinani A, Krispin E, Tadbiri H, Shamshirsaz AA, Espinoza J, et al. Perinatal outcomes of fetoscopic laser surgery for twin–twin transfusion syndrome in triplet pregnancy: cohort study, systematic review and meta-analysis. Ultrasound in Obstetrics & Gynecology. 2022;60(1):42–51.
11. D’Antonio F, Herrera M, Oronzii L, Khalil A. Solomon technique vs selective fetoscopic laser photocoagulation for twin-twin transfusion syndrome: systematic review and meta-analysis of maternal and perinatal outcomes. Ultrasound Obstet Gynecol. 2022 Dec;60(6):731–8.
12. Stirnemann J, Slaghekke F, Khalek N, Winer N, Johnson A, Lewi L, et al. Intrauterine fetoscopic laser surgery versus expectant management in stage 1 twin-to-twin transfusion syndrome: an international randomized trial. Am J Obstet Gynecol. 2021 May;224(5):528.e1-528.e12.
13. Prefumo F, Jauniaux E. Twin-to-twin-transfusion syndrome: from amniodrainage to laser. BJOG: An International Journal of Obstetrics & Gynaecology. 2018;125(9):1163–1163.
14. Senat MV, Deprest J, Boulvain M, Ville Y. Fetoscopic laser surgery versus serial amniodrainage in the management of severe twin-to-twin transfusion syndrome at midgestation. a randomized controlled trial. American Journal of Obstetrics & Gynecology. 2003 Dec 1;189(6):S56.
15. Slaghekke F, Lopriore E, Lewi L, Middeldorp JM, van Zwet EW, Weingertner AS, Klumper FJ, Dekoninck P, Devlieger R, Kilby MD, Rustico MA, Deprest J, Favre R, Oepkes D. Fetoscopic laser coagulation of the vascular equator versus selective coagulation for twin-to-twin transfusion syndrome: an open-label randomised controlled trial. Lancet. 2014 Mar 6. pii: S0140-6736(13)62419-8. doi: 10.1016/S0140-6736(13)62419-8.
16. Roberts D, Neilson JP, Kilby MD, Gates S. Interventions for the treatment of twin-twin transfusion syndrome. Cochrane Database Syst Rev. 2014;1:CD002073.
17. Middeldorp JM, Lopriore E, Sueters M, Klumper FJ, Kanhai HH, Vandenbussche FP, Oepkes D. Twin-to-twin transfusion syndrome after 26 weeks of gestation: is there a role for fetoscopic laser surgery? BJOG 2007;114:694-8.
18. Taylor MJ, Shalev E, Tanawattanacharoen S, Jolly M, Kumar S, Weiner E, et al. Ultrasound-guided umbilical cord occlusion using bipolar diathermy for Stage III/IV twin-twin transfusion syndrome. PrenatDiagn 2002;22:70–6.