New research grant program awards first recipient funding to study methylation in preeclampsia
The Preeclampsia Foundation announces the recipient of the 2018 Peter Joseph Pappas Research Grant, a new grant funding program designed to accelerate preeclampsia research. This first two-year grant, in the amount of $138,696 USD, will be awarded to Kent Thornburg, PhD, and his team at the Center for Developmental Health, Knight Cardiovascular Institute Oregon Health & Science University (OHSU), in Portland, Oregon.
Based on the recommendation of its Scientific Advisory Council, the Preeclampsia Foundation selected Thornburg’s research proposal called “Targeted High-Throughput Methylome Analysis of Early and Late Onset Preeclampsia.” 
Thornburg’s research aims to determine one chemical change in DNA (called methylation) from mothers with preeclampsia and her baby and compare it with DNA from women and babies who did not have preeclampsia. The project will use data from The Preeclampsia Registry to study DNA from women in each of these three groups: those who experienced preeclampsia before 32 weeks’ gestation, after 32 weeks, and women who did not experience the condition. By determining the differences in DNA methylation profiles between women with and without preeclampsia, the research will identify which genes are likely to have made the women vulnerable for acquiring the disease.
Thornburg is the M. Lowell Edwards Chair of Cardiovascular Research, Professor of Medicine, in the Knight Cardiovascular Institute at OHSU. He studies how women adapt to normal pregnancy or to preeclampsia or diabetes, and how the placenta is affected by a variety of diseases. Thornburg also collaborates with scientists around the world, and served as co-chair of the National Institute of Child and Human Development 10-year plan for developmental origins.
Named for the infant son of preeclampsia survivor Lauren Pappas and her husband Clement, the Peter Joseph Pappas Research Grants program will award grants totaling up to $200,000 each year. The ultimate goal of the program is to drive research that will eliminate the delivery of pre-term babies as an intervention for severe preeclampsia, HELLP syndrome, and related hypertensive disorders of pregnancy.
“We lost our son Peter due to preeclampsia following a 29-week delivery in 2015,” explained Lauren Pappas. “Since then we have dedicated our lives to helping others avoid the same outcome by establishing the Peter Joseph Pappas Fund.”
“Thanks to generous contributions from family and friends, and our partnership with the Preeclampsia Foundation, we are making strides to reach our ultimate goal of eliminating pre-term births due to preeclampsia by 2050,” added Clement Pappas.
Thornburg’s research will utilize data available through The Preeclampsia Registry™, the Preeclampsia Foundation’s dynamic database of research participants that includes preeclampsia and HELLP syndrome survivors, family members, and controls (unaffected individuals).
The Peter Joseph Pappas Research Grants program adds to the Preeclampsia Foundation’s portfolio of research programs including the Vision Grant program for young investigators, PRIME for health services research, and EMPOWER, which helps build research capacity in low- and middle-income countries.
If you have any questions about the Peter Joseph Pappas Research Grants program, please email PJPGrants@preeclampsia.org.
Your Participation in Action
 Dr. Sandra Founds from the University of Pittsburgh School of Nursing completed a pilot study to look at a set of genes (genotypes) in DNA and how they relate to the physical symptoms of preeclampsia. Because of your contributions, the Registry was able to provide Dr. Founds with the necessary information.
Dr. Sandra Founds from the University of Pittsburgh School of Nursing completed a pilot study to look at a set of genes (genotypes) in DNA and how they relate to the physical symptoms of preeclampsia. Because of your contributions, the Registry was able to provide Dr. Founds with the necessary information.The study aimed to identify women's symptoms of preeclampsia, such as swelling or headaches, and explore these symptoms with genes that may be linked to preeclampsia (also called "candidate genes"). Over 100 Registry participants with completed enrollment surveys and DNA samples were included in this study. 8 single nucleotide polymorphisms (SNPs), often called "snips", were evaluated in 4 preeclampsia candidate genes. SNPs are genetic differences that can act as biological markers for scientists to learn more about certain conditions. Of the 17 symptoms that were studies, 6 were associated with 4 SNPs, and 7 symptoms were affected in 8 genotypes.
This research learned that certain preeclampsia symptoms can be linked with certain genes, and that it would be reasonable for scientists to consider symptoms in future genetic research of preeclampsia. Future studies to validate these findings could lead to a better understanding of the characteristics of preeclampsia in an effort to better predict, prevent, and provide early precision care to mothers and their babies.
Your help with this study adds another piece to the preeclampsia puzzle, thank you.
Low-Dose Aspirin Continues to Prove Effective in Reducing Onset of Preeclampsia
 A new study recently published by the New England Journal of Medicine found that women at high risk for preterm preeclampsia who took aspirin were less likely to develop the condition than women who were given a placebo.
A new study recently published by the New England Journal of Medicine found that women at high risk for preterm preeclampsia who took aspirin were less likely to develop the condition than women who were given a placebo.Women from 13 different hospitals in seven different countries, who had been identified in their first trimesters as high risk for developing preeclampsia, were randomly prescribed either 150 mg of aspirin or a placebo pill.
In this double blind, prospective study, the aspirin or placebo were administered from 11 to 14 weeks of gestation until 36 weeks in women who were at high risk for preeclampsia.
Study results found that 1.6 percent of women taking the 150 mg dose of aspirin developed preterm preeclampsia, while 4.3 percent of women taking the placebo developed the life-threatening disorder.
Why it matters: Preeclampsia is a critical contributing factor to the loss of mothers and babies during childbirth. As maternal mortality rates continue to rise in the United States, there is increased pressure to find effective treatments for women who are at-risk for preeclampsia. This study is the largest of its kind, including 1,776 randomly assigned women from seven different countries. The study also used the European dose of 150mg, which is almost twice the United States recommended dose of 81 mg. This helps narrow down the effective dose to prescribe and at which point in gestations beginning an aspirin regimen is helpful.
New study reports costs of preeclampsia to the U.S. healthcare system at $2.18 billion in first year
Melbourne, FL -- Eleni Tsigas, Executive Directo of the Preeclampsia Foundation, released the following statement on the American Journal of Obstetrics & Gynecology (AJOG) report on the Short-term costs of preeclampsia to the United States healthcare system:
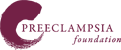
"In this report of major impact, the researchers have documented the short-term medical costs associated with preeclampsia. This aggregated incremental cost was found to be $2.18 billion the U.S. healthcare system for the first 12 months after delivery -- $1.03 billion in maternal healthcare costs and $1.15 billion for infants born to mothers with preeclampsia.
"Total short-term healthcare costs for preeclampsia pregnancies, including the usual costs associated with birth, were estimated to be $6.4 billion, summed across mothers and infants for all gestational ages in the US, so the burden of preeclampsia represents more than one-third of the total costs.
"This is the first and most comprehensive economic analysis to estimate the annual cost burden of preeclampsia for both mothers and infants within the first 12 months after delivery. Quantifying the total cost of a health problem. Preeclampsia, in particular, has been under-recognized and under-researched relative to its prevalence as a leading cause of maternal and infant morbidity and mortality.
"By underscoring the economic burden of preeclampsia, this report provides and important call-to-action for more research funding and awareness of this significant health problem, and a commitment to improving outcomes that focus on prevention, particularly for mothers."
To read the full report, see AJOG's Short-term costs of preeclampsia to the United States healthcare system, and editorial commentary, July 2017.
Community Foundation for Brevard Awards 2015 Medical Research Grant to Preeclampsia Foundation
Melbourne, Florida- The Community Foundation for Brevard has awarded the Brevard-based Preeclampsia Foundation a Medical Research Grant in the amount of $22,500 from the Kenneth R. Finken and Dorothy Hallam Finken Endowment Fund. This grant will extend research funded last year by the Community Foundation to study preeclampsia and its impact on the long-term health of mothers and infants through The Preeclampsia Registry™.
“This grant extends research funded in 2014 to study the genetics of preeclampsia and its association with cardiovascular disease, both of which have dramatic impact on the health of women and children,” said Eleni Tsigas, Executive Director of the Preeclampsia Foundation. “We aim to develop innovative mobile health technology to follow women with prior preeclampsia long-term and to further our genetic studies of the preeclampsia/cardiovascular disease relationship. These efforts will provide an enormous contribution to finding a cause of preeclampsia and to facilitating timely therapeutic intervention for both preeclampsia and cardiovascular disease.”
“This unique medical research with the Brevard-based Preeclampsia Foundation is not only going to benefit mothers and babies world-wide, it also leads to a better understanding of the cause and treatment of cardiovascular disease in women,” said Sandi Scannelli, President/CEO of the Community Foundation for Brevard.
The first of its kind to focus solely on hypertensive disorders of pregnancy, The Preeclampsia Registry captures self-reported and clinical information as well as family and pregnancy history. Overseen by an Institutional Review Board, the registry ensures participants’ privacy and rights in medical research by sharing only de-identified information with approved scientists, researchers, and clinicians.
(From left) Preeclampsia Foundation Executive Director Eleni Tsigas gratefully accepts a
$22,500 medical research grant award from the Community for Brevard’s
Lisa Davidson, Grants & Program Manager, and Community Foundation Board Members
Robert Naberhaus III and Juliana Kreul.
The Preeclampsia Registry tops 2,000; what this means for research
 The Preeclampsia Registry™ has enrolled more than 2,000 participants since its launch in September 2013. Sponsored by the Preeclampsia Foundation, The Preeclampsia Registry is the first of its kind to focus solely on hypertensive disorders of pregnancy, bringing together survivors, family members, and researchers from all over the world. Its purpose is to develop a comprehensive picture of preeclampsia to help discover preventions and treatments, including ones that will reduce the disorder’s long-term health impact.
The Preeclampsia Registry™ has enrolled more than 2,000 participants since its launch in September 2013. Sponsored by the Preeclampsia Foundation, The Preeclampsia Registry is the first of its kind to focus solely on hypertensive disorders of pregnancy, bringing together survivors, family members, and researchers from all over the world. Its purpose is to develop a comprehensive picture of preeclampsia to help discover preventions and treatments, including ones that will reduce the disorder’s long-term health impact.
As the online patient and family database for those affected by preeclampsia and related hypertensive disorders of pregnancy, The Preeclampsia Registry has been designed to aid and accelerate preeclampsia research. Women who have experienced preeclampsia and related disorders may enroll and participate, along with their family members and even friends who were not affected to serve as research “controls”.
The Preeclampsia Registry captures self-reported and clinical information, and family and pregnancy history. We began collecting biological data earlier this year and are completing our current project of sample collection for the registry’s biobank. So far, we have collected more than 500 samples from preeclampsia survivors and their sisters, partners, and children that will help us study preeclampsia’s connection to cardiovascular disease.
Presently, there are six ongoing research initiatives in different phases of completion. One is looking at the genetics of symptoms that women experience, or don't experience. Another will analyze the 'patient journey' from illness to diagnosis to management.
Each participant’s story, medical and pregnancy history, and ongoing health reporting can help scientists unravel the pieces of the preeclampsia puzzle. By allowing us to review your medical records pertaining to preeclampsia, we are able to verify the information you are entering into the registry. This is very important to some research studies. We encourage participants to provide their full medical records and are here to help them make the request to their doctors and/or hospitals. Overseen by an Institutional Review Board, the registry ensures participants’ privacy and rights in medical research at all times.
Participants can view charts and graphs in the "How Did Others Respond?" section on their “My Registry” page and may find data interesting to them. They can find out if other participants experienced the same symptoms or treatments. Because confidentiality is our top priority, no names or identifying information appears on the reports and statistics are displayed as percentages. Participants also have the ability to pose their own research questions in the “My Registry” section of this website.
According to Alina Brewer, Research Coordinator for The Preeclampsia Registry, “There’s a tremendous need for cultural diversity in the registry. Studies are most accurate when they can mirror the population affected by a disease, and increasing our racial and ethnic representation will help investigators gain a better understanding of the characteristics of this disease and validate The Preeclampsia Registry as a valuable resource.”
Participants help create a significant resource for researchers to gather data, start new studies, and make discoveries that will positively affect health outcomes for mothers and babies for many generations to come.
Our goal is to enroll more than 10,000 participants and achieve closer representation of all those affected by hypertension during pregnancy. For more information or to enroll, go to www.preeclampsiaregistry.org or contact Alina Brewer at registry@preeclampsia.org.
Can Pregnancy Complications Predict Future Cardiovascular Risk?
New Rochelle, NY, July 7, 2015—According to a new study, women can accurately recall key pregnancy- related information at least 4 years later that could have important implications for their future risk of developing cardiovascular disease (CVD). A simple and brief questionnaire developed and validated by researchers from Washington University School of Medicine (St. Louis, MO), Harvard School of Public Health, and Brigham and Women's Hospital (Boston, MA) is a valuable new screening tool described in an article in Journal of Women’s Health, a peer-reviewed publication from Mary Ann Liebert, Inc., publishers. The article and an accompanying editorial are available free on the Journal of Women’s Health website until August 7, 2015.
Ebony Boyce Carter, MD, MPH and coauthors assessed the accuracy of the responses to their questionnaire—provided by women who were, on average, more than 4 years postpartum—by comparing the answers to information in the women's medical histories. The pregnancy recall tool includes questions about infant birthweight and length of the pregnancy, and pregnancy-related complications such as gestational diabetes, pre-eclampsia, and pregnancy-associated hypertension. The authors report which pregnancy events and information were more commonly recalled in the article “Pregnancy Complications as Markers for Subsequent Maternal Cardiovascular Disease: Validation of Maternal Recall Questionnaire.”
In the Editorial “Pregnancy as a Window to Cardiovascular Disease Risk: How Will We Know?” Janet M. Catov, PhD, Magee-Womens Hospital (Pittsburgh, PA) says, “The reproductive years are an ideal time to assess pre-clinical CVD risk and launch strategies to prevent or delay onset of disease in women.”
“This brief tool to gather information on pregnancy-related risk factors for future cardiovascular disease can help clinicians identify women at increased risk,” says Susan G. Kornstein, MD, Editor-in-Chief
of Journal of Women’s Health, Executive Director of the Virginia Commonwealth University Institute for Women’s Health (Richmond, VA), and President of the Academy of Women’s Health.
'Get My Health Data' Campaign Launches
Campaign Aims to Remove Barriers, Enhance Demand, and Improve Patient Access to Electronic Health Data
Washington, DC (July 2, 2015) ─ Almost every industry ─ banking, travel, retail, education ─ gives customers powerful tools to manage their lives online. But in health care today, accessing information online is often a confusing and difficult process. Few patients know what to ask for or what information should be available to them, and not nearly enough health care organizations are equipped to meet their requests.
To change that, a diverse and powerful group of patient advocates today launched the Get My Health Data Campaign to support patients in asking for, getting and effectively using their digital health data.
The campaign has three goals: give consumers the information and tools they need to ask for and use their digital health data; identify and promote innovative apps and tools that help consumers securely compile, store and use their health data; and promote a culture in which consumer access to data is the rule, rather than the exception.
“With the Get My Health Data Campaign, we are creating a concerted push from consumers that will liberate digital health information so it gets into the hands of patients and family caregivers, allowing them to more fully engage in their health and care,” said Christine Bechtel, campaign coordinator and advisor to the National Partnership for Women & Families. “Even though we have the technology and policies in place to support patients in accessing their electronic health information, it’s not happening the way it should. Our goal is to enable patients to more easily get and use their digital health information.”
“Over the past five years, doctors and hospitals have widely adopted electronic health records. We’ve declared July 4th ‘Data Independence Day’ because we believe now is the moment when patient demand for their digital health information can flip health care into the open position. Let’s work together to make it practical for people to ask for, share and use their own health data,” added Farzad Mostashari, MD, ScM, former U.S. National Coordinator for Health Information Technology.
More information about the new campaign, including information on how to be successful in requesting data, what to request, patients’ rights to data, resources for providers, and more is available at www.GetMyHealthData.org.
“Too often there are gaps between policy intentions and implementation realities for patients and their families,” said Rebecca Coelius, MD, director of health at Code for America. “We’ve seen that this gap also causes challenges in accessing health data. Code for America has collaboratively built the Vocatus tool to be a simple and free way for patients or their proxies to request medical records, capture whether that request was successful, and provide a feedback loop to health care institutions, the public, and government agencies as part of the Get My Health Data Campaign.”
The Get My Health Data Campaign is coordinated by the National Partnership for Women & Families. Founders include Amida Technology Solutions; Code for America; Genetic Alliance; Health Data Consortium; Farzad Mostashari, MD, ScM; and Aneesh Chopra, former Chief Technology Officer of the United States.
The Preeclampsia Registry Goes Global
Since The Preeclampsia Registry™ was launched in September 2013, the online patient and family database for those affected by preeclampsia and related hypertensive disorders of pregnancy has enrolled more than 1,000 participants. Now one year later, the Preeclampsia Foundation is pleased to announce another major milestone - The Preeclampsia Registry's acceptance into the Global Pregnancy CoLaboratory. Funded by the Bill & Melinda Gates Foundation as part of its PRE-EMPT initiative, this international consortium of databases facilitates research that addresses adverse pregnancy outcomes to improve the health of women and their infants.

The first of its kind to focus solely on hypertensive disorders of pregnancy, The Preeclampsia Registry captures self-reported and clinical information, and family and pregnancy history, and will begin collecting biological data in 2015. Overseen by an Institutional Review Board, the registry ensures participants' privacy and rights in medical research. "The Preeclampsia Registry's partnership with the CoLaboratory is an exciting step forward in advancing preeclampsia research that provides unique data from families and the ability to follow women for many years," said Principal Investigator James Roberts, MD, professor of obstetrics, gynecology, and epidemiology at Magee-Women's Institute & Foundation in Pittsburgh, Pennsylvania, and a member of the Preeclampsia Foundation's Medical Advisory Board. "We are excited to welcome the Preeclampsia Registry to CoLab. This is a valuable addition to our consortium that brings together researchers from all over the world and allows us to share quality clinical data and biological samples, and to facilitate new knowledge generation."
The Preeclampsia Registry is open to anyone who has experienced preeclampsia, eclampsia, HELLP Syndrome, or high blood pressure in pregnancy. Family members are also encouraged to participate. To learn more or enroll, go to www.preeclampsiaregistry.org or emailRegistry@preeclampsia.org.
For more information about the Global Pregnancy CoLaboratory, visit the Pre-EMPT website.
Preeclampsia Doubles Women's Stroke Risk
The estimated 7 million women in the United States today who experienced a hypertensive disorder of pregnancy should be aware of new guidelines for preventing stroke in women from the American Stroke Association and American Heart Association. We have known for many years that a history of preeclampsia during pregnancy puts women at greater risk for future high blood pressure, but continuing research shows that the impact may extend to stroke risk as well.
In the U.S., stroke is now more common in women than men, with more than half of the 795,000 strokes that occur each year happening to women. The disease is also more deadly in women, with about 60 percent of stroke deaths happening in female patients.
"Guidelines for the Prevention of Stroke in Women - A Statement for Healthcare Professionals" from the American Heart Association and American Stroke Association were issued last week. These first-time-ever guidelines, similar to a 2011 publication by the American Heart Association, declared preeclampsia as a significant risk factor for heart disease and stroke. This paper suggested preeclampsia survivors have double the risk of having a stroke and those who de
The guidelines went even farther to recommend interventions to prevent preeclampsia, in the hopes that improved pregnancy outcomes would lower a woman’s risk of stroke. Low dose aspirin and calcium were suggested. [see Box 1] In other research, both of these interventions get mixed reviews, although the former has now been included in the 2013 Hypertension in Pregnancy Guidelines issued by the American College of Obstetricians & Gynecologists. Other research studies on calcium have only found an effect in populations that are calcium-deficient, generally not a problem in the U.S.
Nonetheless, an important part of the conclusions were the recommended follow up actions (see Box 2) which include evaluation and treatment of risk factors as soon as six months after delivery. The ASA guidelines recommend that women with a history of preeclampsia be screened and treated for high 
- Early identification of risk
- Prevention of seizures (eclampsia)
- Control of blood pressure
- Delivery when the magnitude of maternal risk exceeds the interests of the fetus in-utero
- Aggressive postpartum management of fluid status and hypertension
- Surveillance and risk intervention among women affected by preeclampsia as they age
"As advocates for women's health and especially for greater awareness of preeclampsia, we applaud this expression of heightened concern and hope this will lead to much needed research into the cause of preeclampsia and novel treatments," said Eleni Tsigas, Executive Director of the Preeclampsia Foundation. "We are working with a small, but growing body of healthcare providers interested in improving long-term health outcomes for preeclampsia survivors."
Results are in for a major study you made possible!
A major research study using data and DNA samples from The Preeclampsia Registry helps explain the connection between preeclampsia and heart disease. Entitled "Preeclampsia and Cardiomyopathy: Shared Genetics?" this paper was published in Circulation, a well respected peer-reviewed medical journal published by the American Heart Association.
What made this research possible? You! Your ongoing involvement in The Preeclampsia Registry has enabled many other studies which are also underway. "We are sincerely grateful to the women and their families for playing such a pivotal role as we seek to find a cure," said Alina Brewer, Registry Manager.
As you may know, women with a history of preeclampsia are at a two to eight times increased risk of cardiovascular disease (CVD) later in life, however, it isn't fully understood if preeclampsia causes CVD or if the conditions share common risk factors. This study demonstrates that gene variants related to certain types of heart disease, namely idiopathic and peripartum cardiomyopathy, are also associated with preeclampsia. Cardiomyopathy is a condition that makes it difficult for the heart to pump blood to the rest of the body.
This is the largest whole exome sequencing study done on a preeclampsia population. Researchers studied the DNA samples of 181 women with a history of preeclampsia from The Preeclampsia Registry. They conducted DNA sequencing on the samples, looked at variants in the 43 genes known to be associated with cardiomyopathy, and examined the resulting data. The results from The Preeclampsia Registry participants were compared with known results from two control, or comparison, groups.
The study found that women with a history of preeclampsia were significantly more likely to carry a gene variant related to cardiomyopathy that those in the control groups. Different types of variants were examined and reported in the study. For example, when looking at the prevalence of TTN gene-related rare damaging missense variants, these variants were present in 68% of the women confirmed with preeclampsia. This is significantly higher than the control groups that presented 47% and 49% prevalence.
Interestingly, for this subgroup of women, the study found that women with a cardiomyopathy genetic variant were less likely to have had a preterm preeclampsia delivery than those without a variant. Published studies show that women with early-onset preeclampsia are at a greater risk for future cardiovascular disease. However, these results suggest an opportunity to identify risk in women with later onset preeclampsia in order to recommend ongoing follow-up and potential interventions.
Overall, these findings have the potential to better determine a woman's risk for heart disease after preeclampsia and may also inform future studies that seek to define and predict both preeclampsia and heart disease. More research and an improved understanding of the relationship between preeclampsia and heart disease can also influence care during and after pregnancy, and ultimately, improve cardiovascular health for women.
"We've known about gene variants in cardiomyopathy for some time, so we wanted to analyze the presence of these genes among preeclampsia survivors, " said Kenneth Ward, MD, the senior author of the study, medical geneticist, and Laboratory Director at Taueret Laboratories LLC, Salt Lake City, Utah, which provided an in-kind donation to facilitate the sequencing part of this study. "In general, a small number of the general population carry these cardiomyopathy genes, but these preeclampsia survivors had a much higher rate of carrying them."
"This study, and The Preeclampsia Registry more broadly, represent results of a true partnership between preeclampsia, eclampsia, and HELLP syndrome survivors and families, researchers, and the Preeclampsia Foundation," said Eleni Tsigas, the Preeclampsia Foundation's Chief Executive Officer and co-author of the study. "As a patient advocacy organization that empowers survivors and families to drive research, we're pleased to offer The Preeclampsia Registry as an important resource for preeclampsia researchers. In fact, the data resulting from this study will be gifted back to the Registry for other researchers to use."
"Participants in The Preeclampsia Registry are admirably committed to improving preeclampsia outcomes. Their dedication made this study possible and provided insights into preeclampsia and cardiomyopathy genetics that will inform future research with implications for understanding preeclampsia, as well as long-term maternal health," said co-author Hilary Gammill, MD, a Maternal-Fetal Medicine physician-scientist, Associate Professor at the University of Washington, and a co-chair of the Scientific Advisory Council for The Preeclampsia Registry.
Funding for this study was generously provided by the Peter Joseph Pappas Research Grants program through the Preeclampsia Foundation, Taueret Laboratories, LLC, and the Community Foundation for Brevard.
For questions, comments, or to request access to the full manuscript, email registry@preeclampsia.org.
Are you at risk for cardiomyopathy?
You may now be wondering if you are at risk for cardiomyopathy and if individual genetic results are available to you. As stated in the study consent form, we're not able to share individual results from this study. More research needs to be done for healthcare providers to feel confident about using this information to make recommendations for care and treatment. However, this study brings us one step closer to understanding how preeclampsia and heart disease are related. This could not have been done without your help.
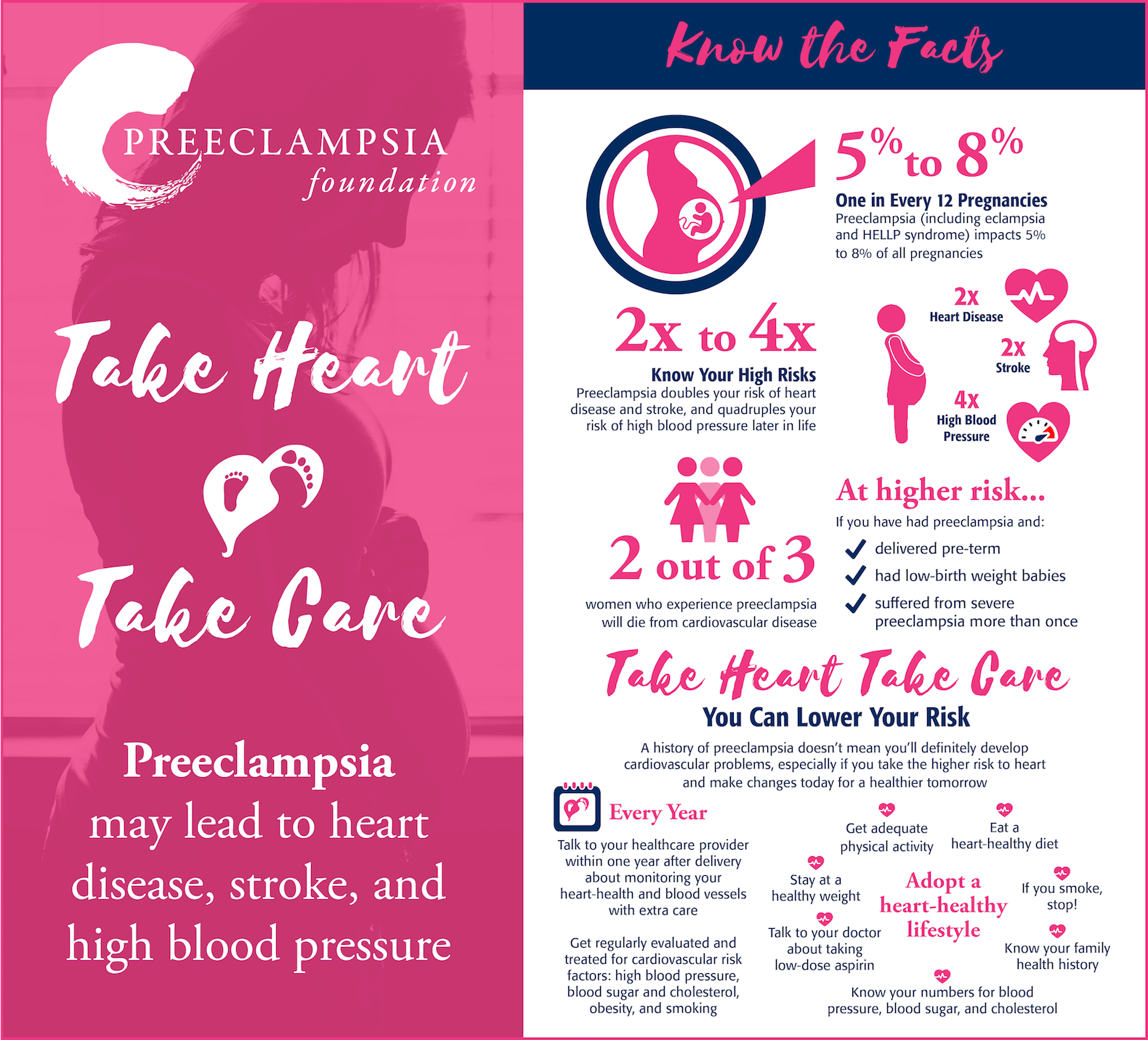
Women that have had preeclampsia have three to four times the risk of high blood pressure and double the risk for heart disease and stroke. They also have an increased risk for developing diabetes. There are, however, things you can do today to minimize your risk. The infographic below explains more.
Will you experience preeclampsia during the next pregnancy?

One of the more frequent questions we hear is “Will I have preeclampsia during future pregnancies? We asked Dr. Ira Bernstein, a member of the Preeclampsia Foundation Medical Advisory Board, to provide some insight.
Most women with a history of preeclampsia have healthy pregnancies in the future. However, there is an increased risk of developing preeclampsia or gestational hypertension in subsequent pregnancies when compared to first pregnancies. Studies have reported recurrence rates for preeclampsia varying from less than 10% to more than 60%, depending on the population studied and the gestational age at onset in the first pregnancy.
A recent analysis on the recurrence of hypertensive disorders of pregnancy showed an overall recurrence rate of 20.7%(1). When looking only at the recurrence of preeclampsia, it was 13.8%. When preeclampsia was diagnosed early in the pregnancy or was more severe there was an increased risk of recurrence. Fortunately, when preeclampsia did recur it tended to be milder and later in onset than in the first affected pregnancy.
Specific high-risk factors, like high blood pressure, diabetes, twin pregnancy, kidney or autoimmune disease significantly increase the risk of preeclampsia recurrence. Other factors that modestly increase the risk of preeclampsia are obesity, maternal age greater than 35, family history of preeclampsia, low socioeconomic status and certain characteristics like African American race. Fortunately low-dose aspirin taken during pregnancy has been shown to decrease the risk of preeclampsia by about 24% in women who are at high risk (2).
Interestingly, women who conceive another pregnancy within a few years following a pregnancy complicated by preeclampsia have a lower risk of having preeclampsia again than if they wait longer to conceive. Also, in the absence of other high-risk factors, the risk for preeclampsia is highest in a woman’s first pregnancy and declines thereafter. Based on these observations, it seems that having a pregnancy, even if it is complicated by preeclampsia, provides some temporary protection from having preeclampsia in the next pregnancy.
One important factor may be the effect of pregnancy itself on a woman’s cardiovascular system. Women studied an average of 14 months postpartum have been shown to have lower blood pressure and more elastic blood vessels when compared to themselves prior to pregnancy. This may represent the modification of important risk factors (3). This effect of pregnancy seems to fade over time, with blood pressure and vessel stiffness returning toward baseline over several years after pregnancy.
An alternative explanation for the increase recurrence of preeclampsia with a longer inter-pregnancy interval is the potential role for new paternity (4). Primipaternity, or a first father effect, also appears to be a risk factor for preeclampsia both in women with a prior pregnancy and women with longer intervals between pregnancies, who have a greater likelihood of having a new partner.
Overall, women who have had a pregnancy complicated by preeclampsia can be optimistic that it is relatively unlikely to happen again. The best protection is to improve modifiable risk factors by maintaining a healthy weight and engaging in regular physical activity, taking low-dose aspirin in future pregnancies and planning future pregnancies within a few years of the first.
Erin Morris, MD
Assistant Professor
Ira M. Bernstein MD
Professor and John Van Sicklen Maeck Chair
Department of Obstetrics Gynecology and Reproductive Sciences
Robert Larner, MD College of Medicine at the University of Vermont
References:
1. van Oostwaard MF, Langenveld J, Schuit E, et al. Recurrence of hypertensive disorders of pregnancy: an individual patient data metaanalysis. American journal of obstetrics and gynecology. May 2015;212(5):624.e621-617.
2. Henderson JT, Whitlock EP, O'Conner E, Senger CA, Thompson JH, Rowland MG. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. Low-Dose Aspirin for the Prevention of Morbidity and Mortality From Preeclampsia: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014.
3. Morris EA, Hale SA, Badger GJ, Magness RR, Bernstein IM. Pregnancy induces persistent changes in vascular compliance in primiparous women. American journal of obstetrics and gynecology. May 2015;212(5):633.e631-636.
4. Robillard PY1, Dekker GA, Hulsey TC.l Primipaternities in families: is the incidence of pregnancy-induced hypertensive disorders in multigravidas an anthropological marker of reproduction? Aust N Z J Obstet Gynaecol. 1998 Aug;38(3):284-7.
New research grant program awards first recipient funding to study methylation in preeclampsia
The Preeclampsia Foundation announces the recipient of the 2018 Peter Joseph Pappas Research Grant, a new grant funding program designed to accelerate preeclampsia research. This first two-year grant, in the amount of $138,696 USD, will be awarded to Kent Thornburg, PhD, and his team at the Center for Developmental Health, Knight Cardiovascular Institute Oregon Health & Science University (OHSU), in Portland, Oregon.
Based on the recommendation of its Scientific Advisory Council, the Preeclampsia Foundation selected Thornburg’s research proposal called “Targeted High-Throughput Methylome Analysis of Early and Late Onset Preeclampsia.” 
Thornburg’s research aims to determine one chemical change in DNA (called methylation) from mothers with preeclampsia and her baby and compare it with DNA from women and babies who did not have preeclampsia. The project will use data from The Preeclampsia Registry to study DNA from women in each of these three groups: those who experienced preeclampsia before 32 weeks’ gestation, after 32 weeks, and women who did not experience the condition. By determining the differences in DNA methylation profiles between women with and without preeclampsia, the research will identify which genes are likely to have made the women vulnerable for acquiring the disease.
Thornburg is the M. Lowell Edwards Chair of Cardiovascular Research, Professor of Medicine, in the Knight Cardiovascular Institute at OHSU. He studies how women adapt to normal pregnancy or to preeclampsia or diabetes, and how the placenta is affected by a variety of diseases. Thornburg also collaborates with scientists around the world, and served as co-chair of the National Institute of Child and Human Development 10-year plan for developmental origins.
Named for the infant son of preeclampsia survivor Lauren Pappas and her husband Clement, the Peter Joseph Pappas Research Grants program will award grants totaling up to $200,000 each year. The ultimate goal of the program is to drive research that will eliminate the delivery of pre-term babies as an intervention for severe preeclampsia, HELLP syndrome, and related hypertensive disorders of pregnancy.
“We lost our son Peter due to preeclampsia following a 29-week delivery in 2015,” explained Lauren Pappas. “Since then we have dedicated our lives to helping others avoid the same outcome by establishing the Peter Joseph Pappas Fund.”
“Thanks to generous contributions from family and friends, and our partnership with the Preeclampsia Foundation, we are making strides to reach our ultimate goal of eliminating pre-term births due to preeclampsia by 2050,” added Clement Pappas.
Thornburg’s research will utilize data available through The Preeclampsia Registry™, the Preeclampsia Foundation’s dynamic database of research participants that includes preeclampsia and HELLP syndrome survivors, family members, and controls (unaffected individuals).
The Peter Joseph Pappas Research Grants program adds to the Preeclampsia Foundation’s portfolio of research programs including the Vision Grant program for young investigators, PRIME for health services research, and EMPOWER, which helps build research capacity in low- and middle-income countries.
If you have any questions about the Peter Joseph Pappas Research Grants program, please email PJPGrants@preeclampsia.org.
What's a registry?
The Preeclampsia Foundation is not a university or research hospital, and like most other patient advocacy organizations, it does not own a state-of-the-art laboratory in which to conduct complicated experiments. However, the Preeclampsia Foundation is a large community of survivors, families, and friends joined in the search for an end to this devastating disorder. With so many questions and theories as to the cause and management of preeclampsia, a patient-driven registry (such as The Preeclampsia Registry) provides survivors and their families an opportunity to play a key role in preeclampsia research.
There are different types of registries that can serve different purposes, but ultimately, a patient registry is a platform to collect information from people who share the same condition and/or have similar experiences. In recent years, patient advocacy and rare disease organizations have become critical contributors to research through patient-driven registries. Often faced with financial barriers, these organizations have sought the most effective avenues to conduct research and create the most impact. Furthermore, these organizations consist of communities of volunteers who are enthusiastic to move research forward, and looking for ways to help, can create a resource unmatched in the clinical research arena.
Participating in a registry will mean answering some questions about your experience with the condition (from a few to over a hundred). Today many registries collect this information over the Internet; however, others may collect this information at a doctor’s office or by phone with a research assistant. Some registries may ask you to provide a copy of your medical records (or permission to release them), and you may also be asked to periodically update your health information.
You may be wondering where this information goes and how it helps to accelerate research. Some researchers just need information (or data) to test their theories, while others also need research participants to enroll in clinical trials. Registries can expedite the research process by providing researchers with valuable information and participants that would otherwise have been more difficult and time consuming to achieve.
The Preeclampsia Registry, for example, provides approved researchers with access to “de-identified” health information – information that does not contain participant names or contact information. This helps researchers to find patterns among preeclampsia survivors that can lead to findings and further studies. Researchers may also pose new questions to a large and willing audience, a strategy that usually takes much longer without a registry.
The Preeclampsia Registry also gives its participants the option of learning about other research studies of which they may qualify and provides them with the means of connecting with these researchers.
Most importantly, patient registries unite the patient voice with clinical research. Patients have questions, theories, and interests that are often different from investigators conducting formal research. By engaging patients in the research process, as we can through patient registries, the chances for discovery and improvement are an even greater possibility.
For more information about patient registries, visit http://www.nih.gov/health/clinicaltrials/registries.htm
To learn more about The Preeclampsia Registry, go to www.preeclampsiaregistry.org